While Russian nuclear medicine specialists are only making overtures towards the theranostics – a blend of both radionuclide diagnostics and targeted therapy for oncological diseases – the technology is already mobilising significant intellectual and financial resources in other countries. Today’s hot spot in theranostics’ world is the prostate cancer; a disease specialists try to diagnose and treat with protein-based radiopharmaceutical agents - prostate-specific membrane antigen (PSMA). Visible success of researchers managed to increase the life expectancy of patients with the prostate cancer up to 3 years, has already caught Big Pharma players’ attention and money – lately last year Swiss Novartis lashed out on specific American start-up costing a whopping $2.1 billion. In Australia, Specialists have been doing Clinical Trials at public expense for the fourth year in the row – at Peter MacCallum Cancer Centre and tens more clinics throughout the country. Vademecum has set activity checkpoints of the matter both in Russia and abroad – and while on its way getting through the topic, asked one of the on-the-scene participants, nuclear medicine specialist, professor Michael Hofman.
- How long has Australia been into theranostics?
- Peter MacCallum Cancer Centre was the first to start making the way to this field. The Centre is the largest government oncology centre in the country. We have been treating rare types of neuroendocrine tumours with Lutetium Lu-177-Dotatate since 2005. Now there are centres in every large city in Australia – Melbourne, Sydney, Brisbane, Adelaide, Perth – performing treatments with Lutetium Lu-177-Dotatate for neuroendocrine tumours. We have treated hundreds of patients with this disease over the years. However, neuroendocrine tumours are very rare so the need is highly specialized. In this last five years the landscape has changed and we have a new target for treating prostate cancer which is a much more common type of tumour. Moreover, it is one of the major causes of death for men with oncological diseases in Australia.
- Did you also start with radionuclide therapy for neuroendocrine tumours?
- Yes. I am a nuclear medicine specialist, I’ve been here at Peter MacCallum for 10 years. I have always liked the diagnostic PET-imaging which has a major impact on patient management, but at the same time I also like the therapeutic aspect of working with radiopharmaceuticals. This is why I first did theranostics of neuroendocrine tumours and then turned to treating prostate cancer, which has now become a focus of my research. I enjoy it a lot. What we have done here is different from other centres doing prostate theranostics, let’s say, in Germany, where individual patients are able to access the therapy, but they have not been producing high-quality data around how effective the treatment is. And that is really what is needed in order to get this treatment accepted by our oncology colleagues and widely available.
- So what is the method about?
- The infrastructure and facilities are the same as for the neuroendocrine tumours, same Lutetium Lu-177 is used as well, but the target is different. We target a molecule called prostate specific membrane antigen, or PSMA, which is highly over-expressed in tumour tissues of prostate cancer. We have developed some small molecules that bind to the Lutetium and then bind very specifically to this receptor which is only expressed on prostate cancer. We also do diagnostics with Gallium-68-PSMA since 2014.
And a year after, in 2015, we started doing therapy with Lutetium Lu-177 PSMA. It is the same molecule, but it is labelled with different radioactive substances. This is how it is done: the Gallium-68 is injected intravenously and finds its way to the prostate cancer by binding to PSMA and it’s been taken up in the prostate cancer cells, it emits a radiation which travels outside of the body, and PET-scanner can detect the radiation, and generate 3-D images. This, by the way, can be done at any stage of cancer. For the treatment, we take a very-very similar molecule, but we label to Lutetium Lu-177 and we inject it intravenously. It is taken up into the same distribution as the Gallium, but the Lutetium only travels 1mm and it emits a different type of radiationcalled Beta-Rays which travel about 1mm. It has very high energy so they can kill the cells that they are taken up to. This is a novel method to deliver very high doses of radiation to prostate cancer cells wherever they happen to be in a body.
- What is the source of funding for these clinical trials?
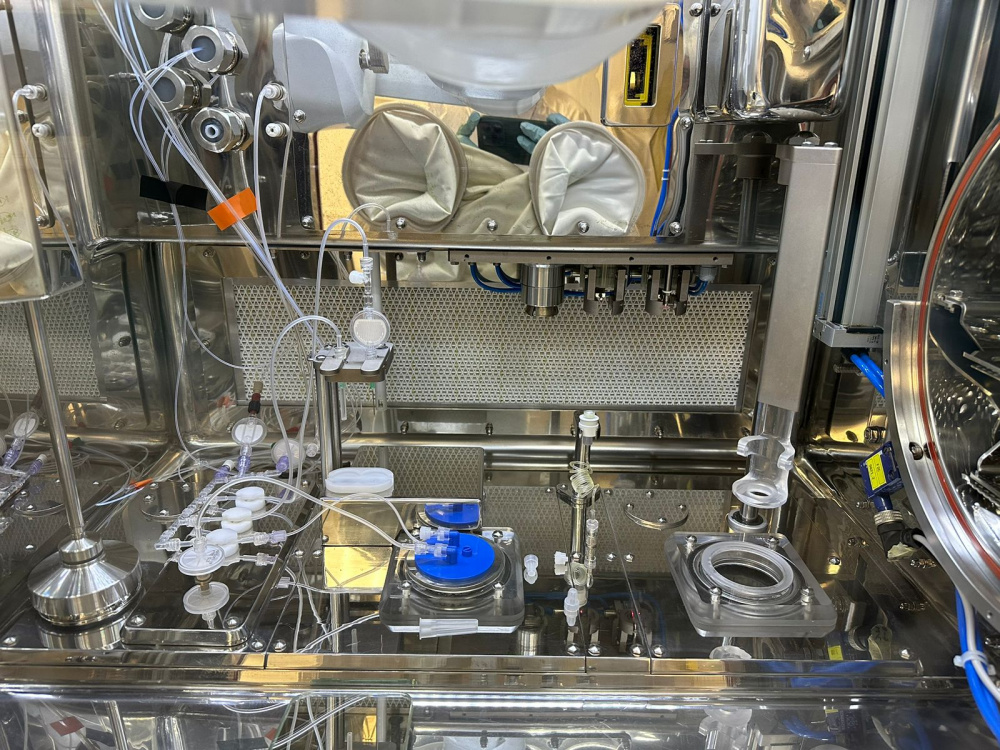
- It did require some intensive effort, we received free supply of the Lu-177 from The Australian Nuclear Science and Technology Organisation, or ANSTO, that make it in Sydney, because they could see the potential market for this treatment in the future, and so they were happy to provide us with free Lutetium for the purpose of the trial, and that’s probably the most costly element of the treatment, the Lu-177. PSMA617, the molecule we are using is manufactured in Germany. This was also supplied to us free. We have a governmental infrastructure here and already have the facilities needed to manufacture it. The only costs necessary to be covered are the salaries but people are already employed, so they just do extra work. And we get patients coming to the hospital, and the actual administration and nursing time is funded by the hospital system. So our situation is quite unique, because it would be very expensive to make such clinical trial from scratch.
So the patients do not pay anything as part of the trial, the only requirement is that they should be the patients of the Peter MacCallum Centre with progressive metastatic castration-resistant prostate cancer. Put simply, it should be Stages IV of prostate cancer, after failing conventional therapy. But this is really where we start, because they are proven therapies and it’s very hard to move a new therapy forward when you have not proved that it works. Now that we have high quality data that works in this really in-stage disease, our focus is now on bringing it earlier and earlier in the treatment phase, but we need to do that in a step-by-step fashion.
- How many patients are now involved in the clinical trial?
- We started this as prospective clinical trial – we treated 30 men initially, and then expanded the trial to 50. These are men who had failed chemotherapy with Docetaxel or some newer generation antigen-hormone drugs that are used including Enzalutamide and Abiraterone These are men who had failed standard therapies and they had really no other options, they would have probably gone to the palliative care with fairly limited survival. And we enrolled them on this trial and treated them and we saw some very good responses, which is what we expected based on the German data that had come before. Now we are running an Australian randomised study We are taking men who have progressed after chemotherapy and the antigen-hormone treatment. We are randomising them to either receive the LuPSMA therapy or a second-line chemotherapy. This is a 200 patient study, it’s being run in 11 centres around Australia. This study commenced around 12 months ago, and it is progressing really well. We have randomised around 130 of 200 patients in the last 12 months, and we should finish recruiting men on this study this year and have results next year.
- In 2018 you stated that in more than half of patients who took part in the trial, PSA level dropped 50% and more. What would it mean from a survival perspective?
- From the 50 patients that we treated initially, we saw about 64% of patients had a dropping their PSA of more than 50%. This is regarded as good or favourable response, and quite a few patients had much deeper responses, PSA drops even down to undetectable levels, but overtime the prostate cancer came back. And the average survival of men that we treated through this 50 patient group was around 13 months, but many men were living much longer than that, particularly the men who had the very good responses. Many of those patients that we treated in 2015 actually are still alive. But without a control arm of the trial it is difficult to put a number on how long we were improving survival, because there is no comparative data.
- How does Lutetium affect quality of life of patients?
- The Lutetium-PSMA is a extremely well tolerated treated because it is very targeted. When we give the radiation, very little goes to normal tissues, almost all of it is taken up into the tumours, so most patients don’t feel unwell at all. In fact they start feeling better, with decreased pain, decreased fatigue,and increased energy. We do see some uptake of the radioactive tracer into the salivary glands, so some people experience dry mouth. This is usually fairly minor; we have never stopped the treatment because of dry mouth. Sometimes we see the blood count drop a little bit. But it is really great, as compared to chemotherapy which has much more severe side effects. And in our further randomised study we will be able to quantify those parameters very well. And from hospital perspective too, you do not need to be admitted to hospital for the treatment.
- Can this be performed as outpatient treatment?
- Australia is strong in nuclear medicine, owing also to the fact that we have very favorable regulations that let us use radioactive molecules on outpatient basis. And here we have some facilities in the hospital for delivering this therapy, which is been specially built as well, cubicles that are lined with some lead shielding so that when we give the Lutetium to the patients, staff around are not exposed to high doses of radiation.P atients come, have the injection, they are quite radioactive for about 4 hours, and we keep them for that period, but after 4 hours the radiation taking up into the tumour and then urinated out, we measure radiation level radioactivity, and then they are safe to go home. Whereas, in Europe, such as in Germany, patients need to stay in hospital for several days, even as long as a week, after this therapy, and it increases the expenses of this therapy considerably. I am not sure the regulations are in Russia.
- Laws are stringent as well.
-. In America it is the FDA that regulates this compounds and they treat them very much like any other drug. And then they get a lot of oversight from FDA and it becomes very difficult to start doing this. In Australia, we are a little bit more deregulated, a lot of these molecules are made onsite in the hospital, and we can give them to patients more easily, which enables us to get the studies up and running or start delivering this treatment.
- How many men would you say are in the need of such treatment?
- It is a large number, it is in the top 4 causes of deaths for men. There is a lot of prostate cancers that are not very aggressive that people die with than rather die from. But there is still a large number of men with more aggressive types of prostate cancer that spreads quite widely that is a lethal condition. So, it is tens of thousands of men in Australia that would be potentially suitable for this therapy once it’s widely available. From a business point of view, it is a large market.
- Has anyone from Big Pharma been interested in this field already?
- More recently, Novartis, one of the big pharmaceutical companies, have bought the rights to this molecule Lu-177-PSMA-617 [through merger of Endocyte for $2.1 bn – VM]. Phase III clinical trials of this molecule are currently away. And since there is a big pharmaceutical company onboard, once they finish their trials, it is expected to become available in the market. If I had to guesstimate, the price would be something in the range of 50,000+ USD for one dose when it’s commercialised. But this is just speculation. That is still cheaper than many other new drugs, or proton therapy.
- Would not it be easier to manufacture the drug in the hospital as you do?
- There’s only about 5 places around the world that make Lu-177. We are lucky to have a local production source of the Lutetium and expertise in handling it in the hospital; it doesn’t currently come delivered in a box. But unfortunately, our way is not for everyone. In the future, this may change as this is commercialised, the final product may be made in bulk and shipped around the world to make it easier. The lutetium actually has a seven-day half-life, so it is possible to make it and send the doses. In the future, probably, in the 5-year time, you would be able to just purchase it and it would get to you in a vial, ready to be injected into patient.
- When the therapy is approved and permitted, will it be covered by Medicare?
- Yes, in reality, it’s not such an expensive treatment, because we give a certain number of cycles and then we stop - so somewhere between 4 and 6 doses of the treatment. I don’t have the exact numbers, but I do not anticipate that this treatment will be more expensive than treatments that exist at the moment, they might actually be cheaper. In fact, in some developing countries, such as India or South Africa, this treatment is available on a fee-for-service basis, and the treatment is cheaper than the drugs, so patients are having this treatment earlier because they are saving money. This might not be the case in other countries.
- Does the scientific world have opinion on experience of India and South Africa since they only sell the service, while others do trials?
- I think in order to get this treatment widely available, we need to get it accepted by our oncology colleagues and other specialists. Without high-level evidence showing that it works and that is better than existing treatments - they will not recommend this treatment to their patients. The sort of evidence they are after is well-designed clinical trials randomised with their competitor around. Without doing the trials, it will never become the mainstream, it would be boutique. Patients will have to find the therapy in the internet and fly to a center, for example, in India. In order to benefit really the population, we need it to be available everywhere, not in one or two centres. And theranostics of prostate cancer have all the chances to become successful.